Revenue Cycle Management
- Home
- Revenue Cycle Management
Revenue cycle management (RCM) refers to the financial process that healthcare providers use to manage the administrative and clinical functions associated with claims processing, payment, and revenue generation. It encompasses all the steps healthcare organizations take to ensure they receive payment for services rendered to patients.
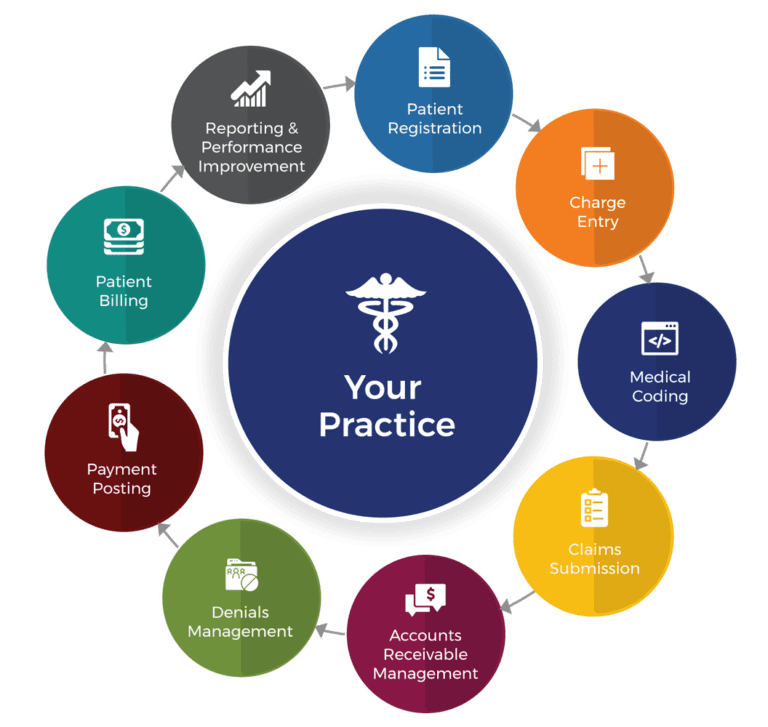
Here’s an overview of the key components and objectives of revenue cycle management:
Patient Registration and Scheduling
This begins the RCM process, where patient demographics, insurance information, and appointment scheduling are recorded accurately to facilitate billing and claims processing.
Insurance Verification
Prior to providing services, healthcare providers verify patients' insurance coverage, ensuring eligibility and understanding coverage limits, copays, deductibles, and any pre-authorizations required.
Coding and Documentation
Healthcare services and procedures performed are documented using standardized medical codes (ICD-10 for diagnoses and CPT/HCPCS for procedures). Accurate coding is crucial for proper reimbursement and compliance.
Charge Capture
Once services are provided, charges are captured based on the documented services and codes. This step ensures all billable services are included for reimbursement.
Claim Submission
Claims are submitted to insurance companies or government payers (like Medicare or Medicaid) electronically or via paper. This process involves attaching necessary documentation and ensuring claims are submitted within required timelines.
Claim Adjudication
Insurance companies review claims for accuracy, completeness, and adherence to coverage policies. They determine the amount payable and either approve, deny, or partially pay claims.
Payment Posting and Reconciliation
Payments received from insurance companies, patients, or third-party payers are posted to patient accounts. Payments are reconciled against billed amounts, adjustments, and contractual allowances.
Denial Management and Appeals
Claims that are denied or underpaid require follow-up and resolution. Healthcare providers may appeal denials with additional documentation or clarification to ensure rightful reimbursement.
Patient Billing and Collections
Patient balances (including deductibles, copays, and non-covered services) are billed after insurance processing. Effective patient billing practices aim to collect outstanding balances promptly while maintaining patient satisfaction.
Financial Reporting and Analysis
Regular reporting and analysis of financial data provide insights into revenue trends, payment patterns, denials, and overall financial performance. This information helps in identifying areas for improvement and optimizing revenue cycle efficiency.
Effective revenue cycle management is essential for healthcare organizations to maintain financial health, optimize revenue capture, reduce billing errors, improve cash flow, and enhance overall operational efficiency. It requires collaboration among clinical staff, billing teams, insurance companies, and patients to ensure timely and accurate reimbursement for healthcare services provided.